MTB 2 : Breast tumor recurrence; Bayes' Theorem
MTB
Molecular Tumor Board 2
Hello all. Today I will start a multi-part MTB that will hopefully initiate discussion as the case progresses. This case will highlight an interesting case, differences between solid tumor NGS and cell-free DNA testing, and the utility of Bayes Theorem in understanding the principles of precision medicine
MTB 2 part 1- MP- History/ Presentation
Breast cancer recurrence
History:
Patient MP
•66 year-old woman with metastatic ductal breast cancer recurrence
•Primary in 2010
•Estrogen Receptor/ Progesterone Receptor (ER/PR), and HER2 positivity on initial Diagnosis
•Recurrence noted 2013 with bone metastases, disease was controlled with 2nd line therapy, although slow progression noted through 2016
•Now (2018) presents with malignant pleural effusion, marked progression noted on PET at involved locations (lymph nodes, bone lesions)
•Latest biopsies from VATS (pleural fluid and mediastial node) shows ER+/PR-, HER2 equivocal by immunohistochemistry, negative by fluorescent in-situ hybridization (FISH)
Treatment Course:
•2010- Xgeva (Donosumab) and Herceptin for primary, showed response for several years
- 2010- prophylactic right total mastectomy with complete axillary dissection
•3rd line, current therapy- Ibrance (palbociclib) and Faslodex (fulvestrant), Herceptin continued:
patient is not currently responding to 3rd line therapy
Pleural biopsy is not thought to have sufficient material for NGS testing by clinician
Clinical Questions submitted to me (as the precision medicine consultant):
- What is the appropriate therapy? Do we discontinue the Herceptin?
TO the Audience:
Thoughts???
- What should be the next course of action? (keep in mind we want to understand patho-mechanisms of disease in precision medicine)
- Bonus Question- what was the likely second line therapy?
MTB 2 Part 2:
Molecular testing results
Molecular testing:
- Because there was not thought to be sufficient cellular material from the pleural effusion, a cell-free DNA test was ordered from a prominent national vendor. This test (ctDNA) identifies mutations from the blood stream.
- After a few weeks the following results were obtained...
- Test results:
- single mutation was identified as relevant
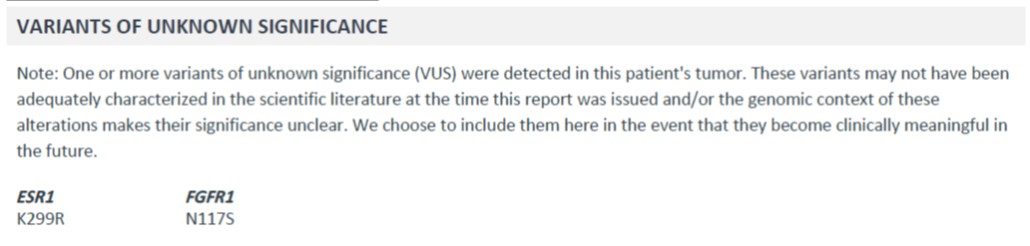
Additionally, the report identifies some other variants:
Questions to be addressed:
- How do these results impact the patient's care?
- What are the advantages and disadvantages of ctDNA compared to solid-tumor FFPE testing?
- What's the deal with VUS (variants of unknown significance)? Why are these reported? Are these somatic variants?
- Bonus Question: What was the likely treatment course given to this patient 2nd line?